In the past I have written about routine as an important element of recovery here "https://bpdlifeinthemoment.blogspot.com/2014/10/routine-bars-of-protection-or.html" For many, one of the most important parts of treatment or therapy, particularly when it lasts a lengthy period of time, is that it provides and external routine on my life. As well as the natural sense of loss at the ending of the therapeutic relationship and important structure is removed at the time of discharge.
Early in the recovery journey I found it difficult not to immediately go back to the routines I had before I asked for help and finally had to give up my job. Problem was the life I thought I was living was completely different. It had to be, after all the way I had been living my life before had led to me becoming completely emotionally and mentally exhausted.
It took me a while and several months during which there were moments when emotional exhaustion returned because I tried to do too much too soon. Any new skills, or routines, no matter how good they will be for me, can take additional mental and emotional effort, simply because I am still becoming used to them.
Be kind to yourself, has to be the refrain - my broken leg, may have had the cast removed, but the muscles around the healing bone need regular practise and exercise to be built up around the bone, in order to make the most of recovery.
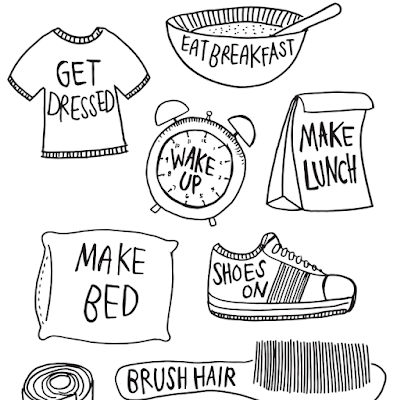
Looking back I think I focused on mastering new and forgotten skills to help me rebuild, in stages. I would identify these now as follows:
1) Keeping 'Body and Soul' together. There are certain tasks, or routines which literally keep us alive. Eating, drinking, sleeping. When beginning to recover from any illness these are essential to keeping the body going, so the mind and emotions can recover effectively. I remember the time when getting out of bed, making regular time for meals and noticing when I was thirsty, actually used up all the energy I had. I would sleep in the middle of the day, because, emotions are exhausting - what told me that this was necessary was the fact that I could still go to bed at a routine time and sleep despite having had naps.
2) Building Self Management. DBT teaches me skills over a sustained period of time. The challenge without the group skills and one to one therapy is to continue to build habits which help me to maintain management of my condition. Because skills such as Emotional Management, Mindfulness and Relationships have routines built into them, the maintenance of them, helps to create a routine in itself.
3) Finding Joy'Glimpses of Glory' is a way a friend of mine heard about last year, when a group of friends were reflecting on the past year just after the Christmas Holidays. Since 2016 when both Brexit and Trump blew onto the world stage, there has been a tendency when reflecting to focus on the negative in the world around us. Instead, looking for 'Glimpses of Glory' encourages us as we reflect to ask that we see the moments of good, the joy we find in the small things in us. When we are rebuilding after a period of illness, we may struggle to see the positive, it can be a symptom of emotional exhaustion. In spite of the fact that I struggle to socialise, I know that there are nurturing relationships and friendships, which I need to build into the fabric of my life. Again, it begins with a small step in opening myself up to friendship....relationships take time to build, but by making meeting up part of my routine, I can begin to make a path out of isolation. To find people who may be good for me, I need to acknowledge the things in life that I enjoy. Where are my Glimpses of Glory....then the next step, are there others who share my joy in these things? It's hard to walk in somewhere new, but when I have a focus, a class, a hobby, a sport, it can help to distract me. It also helps me to connect with the community around me, if I can help in simple ways by volunteering - there are so many opportunities starting with making brews and washing dishes at your local parent toddler group, for example.
These are just small ways that I have rebuilt a routine, which is a safe structure in which to build a new life, where I can manage my condition effectively. Recovery is not a straight line, there have been hiccups and setbacks along the way. But the trend has been towards a more meaningful life for me. Looking back I wasn't ready to move on stage to stage until, the effort needed to maintain new routines has reduced - moving on overlapped at times - life isn't made with beautifully straight edges, like me, the pieces of my routine jigsaw, can be messy!
Reflections on life with BPD. Experience of using DBT to manage ESPD/BPD symptoms. Wanting to connect and encourage others struggling with Mental Illness. Stop the Stigma - the best way to learn about my Mental Health is to ask me about it...
Sunday, 25 November 2018
Sunday, 21 October 2018
Reaching Into the Void
It is one of the most difficult aspects of the emotionally sensitive PD sufferer to communicate. It is a well of undefined emptiness, which seems to endlessly feed my fear of rejection, my sense that I am not made for this world, that life, many times, feels just too hard. It is the cause of so many devastated relationships and friendships, as my need to end the emptiness it brings, swallows up the capacity of those around me to keep loving me.
Recently, I have had the opportunity as a volunteer with lived experience to work alongside staff in a number of co-production projects. Along with the positive I have also had a glimpse at some of the more negative assumptions made about people with a diagnosis of Emotionally Sensitive Personality Disorder, ESPD (also previously known as Borderline Personality Disorder, BPD). Since I was diagnosed seven years ago, I've encountered sudden changes in relationships and friendships, based on ignorance and fear of the label. I have not experienced stigma from professionals who worked directly with me, although many with whom I have shared my treatment journey have told me their own stories of being treated as a 'headache', 'a problem patient', 'manipulative', 'difficult'. I did encounter these attitudes following my diagnosis being added to my medical history, mostly from those in the periphery of my journey, GPs, some A&E staff, those treating me for physical illness.
There is an unspoken expectation that I will be time consuming, difficult and, ultimately that I will not able to be 'boxed off' and 'sorted' by the time my intervention has ended. On reflection I know this does not reflect the compassion of the majority of professionals, but more reflects the lack of ability of the systems and organisation to deal with human beings who have seemingly intractable and complex needs. Our systems are more and more built around outcomes which can be measured and when I present with a complex web of biological and social needs, I mess up the system.
I've spent some time reflecting on the disconnect between the move from 'untreatable' to 'treatable' under the Mental Health Act 2007 and the frustration evident in eye rolling exasperation I can detect in some professionals.
At my worst I could never feel I belonged anywhere. At my worst my emotional pain was so searing and real it felt as if I were walking around with my sternum cracked open. As if it exposed every nerve in my body, pulsing in pain with each beat of my heart so that it felt as if the mere presence of another human in my personal space became unbearable. The core of these feelings centre on a void within which no person could fill.
The sense of helplessness this evokes in those who seek to show me love, often leads to the ultimate breakdown of the relationship as my see-sawing emotions create unending storms. For the person on the receiving end, this see-saw goes from 'love me', to 'I hate you', 'I knew you couldn't love me'. The intensity of loving me can be satisfying for a short time, until the void within swallows every ounce of emotional energy you have to give - many of my relationships ended because of the need of self preservation.
The pressures on the professional working with PD sufferers cannot be easily resolved by an end to the relationship. Indeed, there is a contract, mostly unspoken which says, 'but you can't abandon me, it's your job to care'. I believe from my own observation and experience of positive therapeutic relationships that this is at the heart of the exasperation of many professionals. No individual can possibly remove or fill the void and lack of self which underlies so much of my emotional dysfunction. I have seen the discussions between different agencies who step in to help, or more accurately rescue. After all, when all else fails and I am in so much emotional pain and feel that no one is listening I can always call 999. Police, A&E scoop me up and remove me from all responsibility for managing the void within. I am helped to rest with drugs, I am kept safe by restrictions placed upon me. The reality is that the emptiness remains when the drugs wear off and therefore it becomes a battle to return me to my everyday life.
Where Dialectical Behaviour Therapy (DBT) is different from other interventions is where it asks about my whole life. I need to find an answer to the void within. No one can reach into it for me. For me, meaning and hope come from a personal faith, which helps me to anchor my recovery in a belief that my life has purpose. The challenge for any professional is that the essential question is 'what does a life worth living look like to you?' and means that there is a need to listen to and explore with each individual how they find hope and meaning.
I believe the word 'holistic' is one of those trend words in psychology or medicine which we throw around without exploring to an effective degree what it means in practice. Traditionally, in my experience therapies focus on either my physiology, or my emotions, or thoughts, or all of the above. To be truly holistic we need to look at the core of our being, some would look to spirituality, others might focus on the sense of soul inherent in human relationships. Whatever, when looking at what has worked for me in DBT the difference was in helping me to accept the existence of the void within, whilst encouraging me towards finding out where I could find a sense of belonging and of purpose.
When I consider all of this it is hardly surprising that our longstanding systems and pathways don't fit the needs of the PD sufferer. So we become the 'problem patient', the awkward one that can't be 'treated and streeted'. In essence, though I think there is a need for a different approach for ESPD due to the all pervasive emptiness. I would also say that due to the impact of Mental Illness in general on our physical and spiritual well-being maybe a truly holistic approach to our therapeutic interventions is necessary to help people to rebuild lives with meaning and hope.
Recently, I have had the opportunity as a volunteer with lived experience to work alongside staff in a number of co-production projects. Along with the positive I have also had a glimpse at some of the more negative assumptions made about people with a diagnosis of Emotionally Sensitive Personality Disorder, ESPD (also previously known as Borderline Personality Disorder, BPD). Since I was diagnosed seven years ago, I've encountered sudden changes in relationships and friendships, based on ignorance and fear of the label. I have not experienced stigma from professionals who worked directly with me, although many with whom I have shared my treatment journey have told me their own stories of being treated as a 'headache', 'a problem patient', 'manipulative', 'difficult'. I did encounter these attitudes following my diagnosis being added to my medical history, mostly from those in the periphery of my journey, GPs, some A&E staff, those treating me for physical illness.
There is an unspoken expectation that I will be time consuming, difficult and, ultimately that I will not able to be 'boxed off' and 'sorted' by the time my intervention has ended. On reflection I know this does not reflect the compassion of the majority of professionals, but more reflects the lack of ability of the systems and organisation to deal with human beings who have seemingly intractable and complex needs. Our systems are more and more built around outcomes which can be measured and when I present with a complex web of biological and social needs, I mess up the system.
I've spent some time reflecting on the disconnect between the move from 'untreatable' to 'treatable' under the Mental Health Act 2007 and the frustration evident in eye rolling exasperation I can detect in some professionals.
At my worst I could never feel I belonged anywhere. At my worst my emotional pain was so searing and real it felt as if I were walking around with my sternum cracked open. As if it exposed every nerve in my body, pulsing in pain with each beat of my heart so that it felt as if the mere presence of another human in my personal space became unbearable. The core of these feelings centre on a void within which no person could fill.
The sense of helplessness this evokes in those who seek to show me love, often leads to the ultimate breakdown of the relationship as my see-sawing emotions create unending storms. For the person on the receiving end, this see-saw goes from 'love me', to 'I hate you', 'I knew you couldn't love me'. The intensity of loving me can be satisfying for a short time, until the void within swallows every ounce of emotional energy you have to give - many of my relationships ended because of the need of self preservation.
The pressures on the professional working with PD sufferers cannot be easily resolved by an end to the relationship. Indeed, there is a contract, mostly unspoken which says, 'but you can't abandon me, it's your job to care'. I believe from my own observation and experience of positive therapeutic relationships that this is at the heart of the exasperation of many professionals. No individual can possibly remove or fill the void and lack of self which underlies so much of my emotional dysfunction. I have seen the discussions between different agencies who step in to help, or more accurately rescue. After all, when all else fails and I am in so much emotional pain and feel that no one is listening I can always call 999. Police, A&E scoop me up and remove me from all responsibility for managing the void within. I am helped to rest with drugs, I am kept safe by restrictions placed upon me. The reality is that the emptiness remains when the drugs wear off and therefore it becomes a battle to return me to my everyday life.
Where Dialectical Behaviour Therapy (DBT) is different from other interventions is where it asks about my whole life. I need to find an answer to the void within. No one can reach into it for me. For me, meaning and hope come from a personal faith, which helps me to anchor my recovery in a belief that my life has purpose. The challenge for any professional is that the essential question is 'what does a life worth living look like to you?' and means that there is a need to listen to and explore with each individual how they find hope and meaning.
I believe the word 'holistic' is one of those trend words in psychology or medicine which we throw around without exploring to an effective degree what it means in practice. Traditionally, in my experience therapies focus on either my physiology, or my emotions, or thoughts, or all of the above. To be truly holistic we need to look at the core of our being, some would look to spirituality, others might focus on the sense of soul inherent in human relationships. Whatever, when looking at what has worked for me in DBT the difference was in helping me to accept the existence of the void within, whilst encouraging me towards finding out where I could find a sense of belonging and of purpose.
When I consider all of this it is hardly surprising that our longstanding systems and pathways don't fit the needs of the PD sufferer. So we become the 'problem patient', the awkward one that can't be 'treated and streeted'. In essence, though I think there is a need for a different approach for ESPD due to the all pervasive emptiness. I would also say that due to the impact of Mental Illness in general on our physical and spiritual well-being maybe a truly holistic approach to our therapeutic interventions is necessary to help people to rebuild lives with meaning and hope.
Sunday, 23 September 2018
Spoon Theory and Self Care
Spoon Theory was developed as a way for people with long term life limiting conditions to explain to others who may say, 'but you don't look ill/look ok', how much energy, physical and emotional, it takes just to live day by day. I love it as an easy shorthand between me and those who care to explain how I'm doing on any given day and maybe why on some days I just need to hide away.
The theory is simple. Everyday begins with twelve spoons. Before I plan anything, if I have not slept well, I take one spoon away. If I have missed my meds, or not been keeping to my emotion regulation habits, I take away between one and two spoons. And so on....some days depending on other events which are outside my control I may only start my day with six spoons for everything else in life.
This is particularly useful for helping me with being more compassionate to myself. Perhaps, if I have a social event later in the day I can restock my spoons through positive activities and rest. It helps me feel more objective about how much I can effectively achieve in my day.
It's worth trying to help plan your days. The illustration below gives more ideas about how to calculate and use spoon theory in your day to day self care.
Remember, be kind to yourself!
The theory is simple. Everyday begins with twelve spoons. Before I plan anything, if I have not slept well, I take one spoon away. If I have missed my meds, or not been keeping to my emotion regulation habits, I take away between one and two spoons. And so on....some days depending on other events which are outside my control I may only start my day with six spoons for everything else in life.
This is particularly useful for helping me with being more compassionate to myself. Perhaps, if I have a social event later in the day I can restock my spoons through positive activities and rest. It helps me feel more objective about how much I can effectively achieve in my day.
It's worth trying to help plan your days. The illustration below gives more ideas about how to calculate and use spoon theory in your day to day self care.
Remember, be kind to yourself!
Tuesday, 19 June 2018
Expectations, the NHS and Unintended Consequences
We are proud of our NHS in this country. We rightly celebrate that anyone, no matter what income, or background, can access health services, for free, at the point of need. It is one of the few social contracts which have survived changes of political party and governmental ideology for 70 years. Most of us, recognise the connection between our willingness to contribute through tax and national insurance and the quality of healthcare all within our nation can have access to.
Recently I have been wondering about the unintended consequences of this bastion of the nation's welfare state. I love watching '24 hours in A&E' and more recently, 'Ambulance'. Focusing on the most acute needs and how the public services and people who make up the NHS meet humanity at its often lowest and most vulnerable point of need. At its best these television programmes show the dedication and endless compassion and professionalism of our doctors, nurses, porters, paramedics. Bizarrely, you may think, I find both of these programmes uplifting.
From time to time, though there is the exposure of an element of disdain from some of those phoning for emergency help. 'Where is the (expletive) ambulance? I've fallen over...', 'are you breathing?'....'*@!&ing get me some help....', 'Are there any injuries, are you bleeding, are you in a vulnerable position, are you or anyone with you at immediate risk of serious injury or death?', 'No, but you have to sort me out...' and so the demands go on, with long suffering Control Centre staff dealing with the abuse whilst watching the lights flash as serious emergencies build up, requiring response. Perhaps, this demonstrates the truth that familiarity - and availability breed contempt?
Before I was finally diagnosed and was able to access some very good Mental Health Services, locally - flawed and imperfect, but to me an absolute lifesaver! - I remember being contacted via the magic of t'interweb by a former student from my days teaching A Level English. She had qualified as a Neuro Scientist and had secured a post doing research at Harvard. Our email exchanges were enjoyable discussions of my fresh understanding of my own condition and some really interesting research she was involved in to do with brain structures, the limbic system and the impact on mental illness. However, naturally the discussion also included our experiences of accessing health in the USA and UK respectively.
I had received a number of different referrals, starting with my GP who had worked with me to explore beyond an acceptance my 'over-emotional' responses as anxiety and depression, the treatment for which seemed to only offer temporary relief from the patterns identified in my medical history. I was referred to specialist practitioners and consultants until we arrived at a diagnosis which led to a treatment pathway. Most of all, even though it was a label, what it gave to me was a way to understand the pervasive symptoms which had plagued me all my life.
The waiting times in 2011 had not suffered much from cuts in services so waiting times for appointments varied from two weeks to nearly a year. Despite having to wait at different stages, at no time following diagnosis was I left 'adrift', I maintained weekly appointments with my CPN and monthly appointments with my GP until the treatment I was offered had a place for me. Following five years of consistently good care, (there was the odd disappointment along the way), I was discharged with the skills I needed to manage my condition. Thankfully at no point was I forced to weigh up treatment options based on what was left in my bank account (very little as it happens).
My former student, though, shared with me that although she had very good medical insurance provided by her employer, was facing a $50,000 bill following hospitalisation after she had been involved in a serious car accident which led to her being in hospital for four weeks. The bill was for the portion of treatment not covered by her insurance.
So yay for the NHS. However, I have observed in myself along the way some attitudes which could loosely be described as 'learned helplessness' - simply because if I have any little concern about my health all I have to do is book an appointment online or by phone (forget the waiting time) for free to get it checked out. This is where our expectations and the realities of the limits of any therapy (physical or mental health related) clash. Because of the ease with which we can ask for help, I think we can sometimes confuse this with the abilities of any intervention to undo the ravages of time and/or trauma whether physical, emotional or mental. With this mind set I begin my journey towards therapy with an assumption that the professional in front of me is embued with some magical 'fairy' dust called 'The NHS Magic Dust' which they can sprinkle on my area of need and immediately bring about healing.
An unintended consequence of the availability of free healthcare is that when I am prescribed a therapy or medical intervention which requires effort and discomfort to myself, I either ignore the prescription or try it half-heartedly or for a limited amount of time before declaring the NHS 'useless' and unable or (worse) unwilling to help me. I remember my GP telling me about patients who had been referred for physiotherapy to help alleviate longstanding physical pain. Some would return to her having completed all the Physio appointments with the news that 'it hasn't helped'. On exploring further, my GP would discover that the patients perceived the therapy to be limited to six, weekly appointments with the therapist without taking the exercises home and practising them on a daily and ongoing basis.
The first thing that made me pause for thought following my diagnosis and referral to DBT (Dialectical Behaviour Therapy) was the initial meeting with my therapist when she made clear to me that she could not stop my distress, nor could she remove the emotional pain I was experiencing. However, what I was offered was hope that TOGETHER we could work to develop skills and practises which would eventually help me to manage my condition.
I recognise why A&E staff groan when presented with someone in emotional or mental distress. If I turn up with an obvious physical wound, you can offer me support and even the means to lessen or remove the pain I am feeling.
I wonder if another unintended consequence of the NHS is in regard to our Mental Health more than our physical health. I have blamed the failings of the NHS for not providing a personally tailored solution to the complex emotional and mental challenges caused by a combination of my biology and my experiences of life. Looking at it in black and white prompts me to ask myself: 'who told you, you were the centre of the universe and the focus of all public health efforts?' It also begs the question - without referring to that other Dr - who could possibly undo my brain structures and the impact of my limbic system, or the impact of my life experiences on both of those? Certainly no earthly physician - as far as I know. Yes antibiotics have managed to help us eradicate the threat of bacterial infections. However, I am often reminded of how simple those 'germs' are as organisms compared to human beings. More than any other aspect of our health, our mental and emotional health requires that we are fully engaged and involved in both understanding and managing the struggles that we face.
A Sea-Change in attitude is emerging - a recognition that medicalising and medicating mental health is not effective as an approach, in isolation. As a complex being, I probably am likely to respond better to interventions which see me as an integrated and whole human being, rather than focusing on my challenges in isolation. 'I am not my diagnosis' resounds.
I hope that as we move forward we do so as patients and professionals joining forces to find the best outcomes for each person in need. After all, the NHS cannot possibly be present for the 95% of my life which is where I am fighting the majority of my battles against ill health. If I can do all I can to help myself as much as I can, then maybe I can leave the NHS and its precious resources for when I really need it and therefore release more resources for those who are in urgent need right now.
Recently I have been wondering about the unintended consequences of this bastion of the nation's welfare state. I love watching '24 hours in A&E' and more recently, 'Ambulance'. Focusing on the most acute needs and how the public services and people who make up the NHS meet humanity at its often lowest and most vulnerable point of need. At its best these television programmes show the dedication and endless compassion and professionalism of our doctors, nurses, porters, paramedics. Bizarrely, you may think, I find both of these programmes uplifting.
From time to time, though there is the exposure of an element of disdain from some of those phoning for emergency help. 'Where is the (expletive) ambulance? I've fallen over...', 'are you breathing?'....'*@!&ing get me some help....', 'Are there any injuries, are you bleeding, are you in a vulnerable position, are you or anyone with you at immediate risk of serious injury or death?', 'No, but you have to sort me out...' and so the demands go on, with long suffering Control Centre staff dealing with the abuse whilst watching the lights flash as serious emergencies build up, requiring response. Perhaps, this demonstrates the truth that familiarity - and availability breed contempt?
Before I was finally diagnosed and was able to access some very good Mental Health Services, locally - flawed and imperfect, but to me an absolute lifesaver! - I remember being contacted via the magic of t'interweb by a former student from my days teaching A Level English. She had qualified as a Neuro Scientist and had secured a post doing research at Harvard. Our email exchanges were enjoyable discussions of my fresh understanding of my own condition and some really interesting research she was involved in to do with brain structures, the limbic system and the impact on mental illness. However, naturally the discussion also included our experiences of accessing health in the USA and UK respectively.
I had received a number of different referrals, starting with my GP who had worked with me to explore beyond an acceptance my 'over-emotional' responses as anxiety and depression, the treatment for which seemed to only offer temporary relief from the patterns identified in my medical history. I was referred to specialist practitioners and consultants until we arrived at a diagnosis which led to a treatment pathway. Most of all, even though it was a label, what it gave to me was a way to understand the pervasive symptoms which had plagued me all my life.
The waiting times in 2011 had not suffered much from cuts in services so waiting times for appointments varied from two weeks to nearly a year. Despite having to wait at different stages, at no time following diagnosis was I left 'adrift', I maintained weekly appointments with my CPN and monthly appointments with my GP until the treatment I was offered had a place for me. Following five years of consistently good care, (there was the odd disappointment along the way), I was discharged with the skills I needed to manage my condition. Thankfully at no point was I forced to weigh up treatment options based on what was left in my bank account (very little as it happens).
My former student, though, shared with me that although she had very good medical insurance provided by her employer, was facing a $50,000 bill following hospitalisation after she had been involved in a serious car accident which led to her being in hospital for four weeks. The bill was for the portion of treatment not covered by her insurance.
So yay for the NHS. However, I have observed in myself along the way some attitudes which could loosely be described as 'learned helplessness' - simply because if I have any little concern about my health all I have to do is book an appointment online or by phone (forget the waiting time) for free to get it checked out. This is where our expectations and the realities of the limits of any therapy (physical or mental health related) clash. Because of the ease with which we can ask for help, I think we can sometimes confuse this with the abilities of any intervention to undo the ravages of time and/or trauma whether physical, emotional or mental. With this mind set I begin my journey towards therapy with an assumption that the professional in front of me is embued with some magical 'fairy' dust called 'The NHS Magic Dust' which they can sprinkle on my area of need and immediately bring about healing.
An unintended consequence of the availability of free healthcare is that when I am prescribed a therapy or medical intervention which requires effort and discomfort to myself, I either ignore the prescription or try it half-heartedly or for a limited amount of time before declaring the NHS 'useless' and unable or (worse) unwilling to help me. I remember my GP telling me about patients who had been referred for physiotherapy to help alleviate longstanding physical pain. Some would return to her having completed all the Physio appointments with the news that 'it hasn't helped'. On exploring further, my GP would discover that the patients perceived the therapy to be limited to six, weekly appointments with the therapist without taking the exercises home and practising them on a daily and ongoing basis.
The first thing that made me pause for thought following my diagnosis and referral to DBT (Dialectical Behaviour Therapy) was the initial meeting with my therapist when she made clear to me that she could not stop my distress, nor could she remove the emotional pain I was experiencing. However, what I was offered was hope that TOGETHER we could work to develop skills and practises which would eventually help me to manage my condition.
I recognise why A&E staff groan when presented with someone in emotional or mental distress. If I turn up with an obvious physical wound, you can offer me support and even the means to lessen or remove the pain I am feeling.
I wonder if another unintended consequence of the NHS is in regard to our Mental Health more than our physical health. I have blamed the failings of the NHS for not providing a personally tailored solution to the complex emotional and mental challenges caused by a combination of my biology and my experiences of life. Looking at it in black and white prompts me to ask myself: 'who told you, you were the centre of the universe and the focus of all public health efforts?' It also begs the question - without referring to that other Dr - who could possibly undo my brain structures and the impact of my limbic system, or the impact of my life experiences on both of those? Certainly no earthly physician - as far as I know. Yes antibiotics have managed to help us eradicate the threat of bacterial infections. However, I am often reminded of how simple those 'germs' are as organisms compared to human beings. More than any other aspect of our health, our mental and emotional health requires that we are fully engaged and involved in both understanding and managing the struggles that we face.
A Sea-Change in attitude is emerging - a recognition that medicalising and medicating mental health is not effective as an approach, in isolation. As a complex being, I probably am likely to respond better to interventions which see me as an integrated and whole human being, rather than focusing on my challenges in isolation. 'I am not my diagnosis' resounds.
I hope that as we move forward we do so as patients and professionals joining forces to find the best outcomes for each person in need. After all, the NHS cannot possibly be present for the 95% of my life which is where I am fighting the majority of my battles against ill health. If I can do all I can to help myself as much as I can, then maybe I can leave the NHS and its precious resources for when I really need it and therefore release more resources for those who are in urgent need right now.
Wednesday, 18 April 2018
Recovery Story
I have been asked to tell my story at a conference of the World Association for Psychiatric Recovery at the end of April. As part of the preparation I was also asked to provide a written version for delegates to take away...this is it:
‘The past is a foreign country.’ Not for me. My emotional memory is highly tuned and sensitive to pain and suffering, which means that the memory of childhood trauma can hold the same emotional impact 30 or 40 years later as the moment it happened. I did not know that my emotional and mental battles had a name until I was 42 years old. I had first been referred for support from mental health services, by my teachers at the age of 16.
I was the classic ‘quiet child’. I didn’t cry, I did not speak in groups, did not speak in school, communicating with adults through my brother or a close childhood friend who started school with me at the age of 4. My brother and I suffered similar, significant physical and emotional abuse. For me this was compounded by sexual abuse from a series of perpetrators until the age of 18 when I finally escaped to university. School was my safety, literature was my escape, although until an inspiring teacher noticed me when I was aged 9, my first school labelled me as educationally, ‘sub-normal’, despite the fact I was devouring books at home.
Despite our similar family experiences my brother and I have managed to live as adults with very different outcomes. He has never suffered any significant mental health issues. Here is where my brain reacts differently to the world from those around me. I have been given a number of labels since 2011 when it was first suggested by an assessment, following persistence from my GP that my symptoms and mental health history indicated a diagnosis of Borderline Personality Disorder (BPD). I know many patients find this label problematic, but, given the fact that I had successfully sidestepped hospitalisation despite entrenched patterns of self-harm and suicidal ideation, I viewed the news as an opportunity to move forward.
By 2011 I had been working as a Probation Officer for nearly ten years. I specialised in Domestic Abuse cases as well as those who were considered ‘untreatable’ by Mental Health professionals due to ‘Personality Disorder’ diagnosis. By 2007 the Mental Health Act stopped this loophole and stated that professionals could no longer pass the buck to Criminal Justice Agencies where prison certainly was not the appropriate setting in which to address both self-destructive and violent behaviours. I was able to work within a multi-disciplinary team, made up of Probation, Police, NHS and voluntary sector staff to address the key socio-economic factors, alongside mental health and addiction issues, in order to address offending behaviour. It was within this context that I first came across the work of Marsha Linehan in developing a specific therapeutic approach to BPD patients which has become the Dialectical Behaviour Therapy (DBT) model.
I recognised how effective DBT could be for some of our cases when set in the context of significant community support. Unfortunately, 2010 brought a new government who did not feel able to support such ‘end to end’ management of offenders with a rehabilitative continuum supporting people as they moved from prison and sought to re-integrate effectively within their communities.
All of this experience meant I was open to the possibilities offered to me by DBT to develop the skills necessary to manage the impact of my past whilst learning about my emotions and the impact of the world around me on my mental health. I recognised that having learned about emotions, DBT would offer me new coping skills to manage my emotions more effectively than all the self-destructive behaviours I had previously employed to ’survive’ life. I was grateful that my diagnosis came at the same time that LCFT started to deliver DBT as a pathway for BPD.
In telling my story I am keen to identify the factors within DBT and the Wellness Recovery Action Planning (WRAP) programme which have been instrumental in helping me to maintain my mental and emotional wellness.
1. Managing Expectations – Often I have observed in professionals a natural tendency to recoil from the levels of distress I have expressed when I am in crisis. My label has recently changed on my records from BPD to ESPD (Emotionally Sensitive Personality Disorder). It does not fully explain the complex mix of biology and social environments which result in me displaying extreme reactions to the world around me. It is Marsha Linehan who has articulated for me, the extent of my emotional distress:
‘Borderline individuals are the psychological equivalent of third-degree-burn patients. They simply have, so to speak, no emotional skin. Even the slightest touch or movement can create immense suffering.’
For the professional who encounters such apparent suffering, there is an almost unbearable pressure which seems to come from me, in despair crying, ‘help me’. This is where the professionals’ role in recovery perhaps needs to be adjusted, and I would suggest, is within the DBT model.
In my first meeting with my one to one therapist and the DBT Contract signed by me and my therapist, there is an acknowledgement that no human being, no matter how skilled, can stop me from feeling the pain of my life in the past, nor can they give me a prescription which immediately removes or dulls emotional pain. What I am offered is hope that together we can work to help me learn to manage my distress, make friends with my emotions and make changes to the behaviour which so far has served to prolong my suffering.
Throughout my experience of DBT I was encouraged to attend ‘training sessions’ (Group Skills) and apply those skills with the help of my DBT therapist (my ‘Coach’) to my own life. The question which after decades opened the door on hope for me, having ‘failed’ at numerous talking therapies, was ‘What does a life worth living look like for you?’ I was informed that no treatment or professional can undo my past experiences, nor can one person or therapy undo decades of maladaptive coping mechanisms in a limited period of time and within solely clinical settings. As with referrals to Physiotherapy for those with physical injuries, recovery means that there is a responsibility on the patient to take the exercises learned and practise them in the real life setting.
2. Managing Limits – From the beginning of the DBT therapeutic relationship, there is a clarity and agreement that both patient and professional will have their own personal and professional limits - it is helpful if an agreement is made about what those limits are and what the likely consequences of breaching those limits will be. There is also an understanding that each therapist has the backing of a team who understand and agree with the ethos of the DBT approach. This provides protection for both the patient and the therapist. In terms of carrying it into real life this models protective boundaries necessary to keep relationships going.
In the past my life patterns seemed to go in five year cycles. Every five years my central relationships would not only end, but explode with all kinds of collateral damage, resulting usually in a loss of accommodation and employment. I would spend some time in treatment, recovering, usually travelling abroad, in extreme settings (ie war zones), then restarting in a new location. Now I am building up a strong network of friends in a place I have lived and worked in for 16 years. When I was first diagnosed I was socially isolated and unable to find the emotional strength to start to build relationships outside myself and those necessary for a job to work.
3. Managing Reality – When struggling with the basics of life, usually most forcefully at the beginning of the recovery journey, before diagnosis, there is a perception that I am the only one experiencing life in this way. I have a distorted view of the levels of my own failures. In a sense I believe I was like Supergirl, not only did I feel I was an alien on earth, I also expected of myself massively higher standards and limits than anyone else. Until, ESPD became my ‘Kryptonite’ reminding me that after all I am flawed and human, and therefore absolving me of responsibility for everything bad in the world. In short, as I was reminded during my DBT journey, the universe doesn’t actually revolve around me and there are many, oh so many, things I do not and cannot control.
Another reality that comes as a shock after years of trying to manage a daily rollercoaster ride of extreme feelings is that, most of everyday life is boring and uninspiring - when struggling with Mental Health issues there can be a distorted view of life on the 'other side' where life must be rosy, easy and better than that experienced by me.
This is where involvement in real communities, becomes essential to maintaining recovery. If I can only relate to those who have an experience of Mental Health Services, or who have a shared diagnosis, then I am not allowing myself to experience the variety of relationships around me. It is more positive and more akin to real life to join groups which are focused on a location, sport, or interest. I have developed a ‘wellness group’ which, after nearly 3 years is firmly established within a defined local community. This means that we offer not only a weekly group focused on a programme to help us engage with activities which are available locally and can help our mental, physical and spiritual wellness. We have a strong online community of over 100 people who have come through word of mouth. We recognise that people are on a different part of the recovery journey so our weekly group is flexible and adapts to the needs of the group membership. As such we do not have a static membership, some people attend during sickness absences from work as a support in returning to work and move on. Some attend not knowing much about how to ask for help and need signposting and practical support to access GP referrals. Some are carers. Since we began we have had 50 members of the weekly group with this year’s group running at 6-8 people attending each week. We also meet on a one to one basis to provide signposting and advice, contact is usually made via local community contacts or by Direct Message on our Facebook page.
We encourage people to move out from our group and try other community involvement through our contacts with local groups and businesses. Having the opportunity to contribute within a wider community is vital to recovery. There is such a thing as a meaningful life - this cannot include unlimited access to Mental Health services as that is not the experience of most people. There is something intrinsically unhelpful if the only safe places a person feels they have can only be within Mental Health services or in socialising with those who have similar experiences. This is different from peer support.
4. Managing Discharge – From day one the end of DBT therapy and discharge were discussed openly with me, even though my actual date of discharge was nearly two years away, I was preparing for it from the moment I started therapy. Unlike my previous experience of endings I was more than ready to move forward, even though I was not symptom free I was able to leave feeling confident that I could live with the limits caused by my ‘Kryptonite’.
5. Managing my condition - Everyone has the ability to manage their condition if provided with the right skills and therapy to help them build a meaningful life in spite of their diagnosis. Hope is always there from day one underpinning the efforts of both staff and patients.
A Word about Relapse
I was discharged from the Complex Care and Treatment Team in 2014. In April 2017 I suffered a relapse in my condition requiring the intervention of the Crisis Team and Home Treatment Team. This had been triggered by financial pressures caused by a 2/3 cut in my benefits. Apart from not having enough for food and utilities this could have resulted in the repossession of my home. Thankfully the work I had put into building strong relationships meant that some friends were able to buy a percentage of my house and secure my residence. At the same time, it was taking 18 months to appeal the assessment decision. Each stage in the appeals procedure was highly distressing and only ended in October 2017 when I had to present my case to a panel at the Magistrates’ Court. Sometimes the environment is too powerful for me to manage even with my DBT skills.
I did feel like a failure, but I was told the DBT team within LCFT had developed the Acute Therapy Service (ATS) which helped me to stay in my home with the support of the HTT and my social network. I travelled to the ATS unit daily and for six days was given respite from the relentless pressures, to sharpen my mindfulness and emotion management skills. It felt like I was able to reboot and return to the same pressures but with my hope restored.
When you have been on the recovery pathway for some time, relapse can feel devastating until I take a step back and recognise how far I’ve come. The skills I once relied on to prevent self-harm are no longer required, but other sets of DBT skills are habitual, particularly mindfulness.
Hope and Meaning
Hope and Meaning cannot properly be provided by medication or therapy within a clinical setting. For me, hope and meaning come from a personal faith in a God who is bigger than me and my past and problems. For anyone, whatever their belief system finding someone or something that is bigger is important to providing an answer to the question, ‘What do you get up for each day?’ I think that the journey through therapy can partly be a search to discover what this is for each individual. It’s important for me to know why I should comply or co-operate with interventions or medications. In the past when I was unable to find an appropriate answer I was the nightmare patient – ‘uncooperative’ and ‘disruptive’.
I have long held that all of life is a journey, we pass through different terrain and places. Along our life’s journey we may be joined by others who travel the same path. I have seen those who have helped me as Care Co-ordinators, Therapists and Facilitators as ‘journey friends’, people who join me for a part of the journey. Some, the best practitioners, walk alongside me. Others, run ahead, leaving me lagging behind. Others, stay behind me, out of sight, making me feel uneasy and judged.
I am grateful for a therapeutic pathway which offered me hope that things could be different one day.
‘The past is a foreign country.’ Not for me. My emotional memory is highly tuned and sensitive to pain and suffering, which means that the memory of childhood trauma can hold the same emotional impact 30 or 40 years later as the moment it happened. I did not know that my emotional and mental battles had a name until I was 42 years old. I had first been referred for support from mental health services, by my teachers at the age of 16.
I was the classic ‘quiet child’. I didn’t cry, I did not speak in groups, did not speak in school, communicating with adults through my brother or a close childhood friend who started school with me at the age of 4. My brother and I suffered similar, significant physical and emotional abuse. For me this was compounded by sexual abuse from a series of perpetrators until the age of 18 when I finally escaped to university. School was my safety, literature was my escape, although until an inspiring teacher noticed me when I was aged 9, my first school labelled me as educationally, ‘sub-normal’, despite the fact I was devouring books at home.
Despite our similar family experiences my brother and I have managed to live as adults with very different outcomes. He has never suffered any significant mental health issues. Here is where my brain reacts differently to the world from those around me. I have been given a number of labels since 2011 when it was first suggested by an assessment, following persistence from my GP that my symptoms and mental health history indicated a diagnosis of Borderline Personality Disorder (BPD). I know many patients find this label problematic, but, given the fact that I had successfully sidestepped hospitalisation despite entrenched patterns of self-harm and suicidal ideation, I viewed the news as an opportunity to move forward.
By 2011 I had been working as a Probation Officer for nearly ten years. I specialised in Domestic Abuse cases as well as those who were considered ‘untreatable’ by Mental Health professionals due to ‘Personality Disorder’ diagnosis. By 2007 the Mental Health Act stopped this loophole and stated that professionals could no longer pass the buck to Criminal Justice Agencies where prison certainly was not the appropriate setting in which to address both self-destructive and violent behaviours. I was able to work within a multi-disciplinary team, made up of Probation, Police, NHS and voluntary sector staff to address the key socio-economic factors, alongside mental health and addiction issues, in order to address offending behaviour. It was within this context that I first came across the work of Marsha Linehan in developing a specific therapeutic approach to BPD patients which has become the Dialectical Behaviour Therapy (DBT) model.
I recognised how effective DBT could be for some of our cases when set in the context of significant community support. Unfortunately, 2010 brought a new government who did not feel able to support such ‘end to end’ management of offenders with a rehabilitative continuum supporting people as they moved from prison and sought to re-integrate effectively within their communities.
All of this experience meant I was open to the possibilities offered to me by DBT to develop the skills necessary to manage the impact of my past whilst learning about my emotions and the impact of the world around me on my mental health. I recognised that having learned about emotions, DBT would offer me new coping skills to manage my emotions more effectively than all the self-destructive behaviours I had previously employed to ’survive’ life. I was grateful that my diagnosis came at the same time that LCFT started to deliver DBT as a pathway for BPD.
In telling my story I am keen to identify the factors within DBT and the Wellness Recovery Action Planning (WRAP) programme which have been instrumental in helping me to maintain my mental and emotional wellness.
1. Managing Expectations – Often I have observed in professionals a natural tendency to recoil from the levels of distress I have expressed when I am in crisis. My label has recently changed on my records from BPD to ESPD (Emotionally Sensitive Personality Disorder). It does not fully explain the complex mix of biology and social environments which result in me displaying extreme reactions to the world around me. It is Marsha Linehan who has articulated for me, the extent of my emotional distress:
‘Borderline individuals are the psychological equivalent of third-degree-burn patients. They simply have, so to speak, no emotional skin. Even the slightest touch or movement can create immense suffering.’
For the professional who encounters such apparent suffering, there is an almost unbearable pressure which seems to come from me, in despair crying, ‘help me’. This is where the professionals’ role in recovery perhaps needs to be adjusted, and I would suggest, is within the DBT model.
In my first meeting with my one to one therapist and the DBT Contract signed by me and my therapist, there is an acknowledgement that no human being, no matter how skilled, can stop me from feeling the pain of my life in the past, nor can they give me a prescription which immediately removes or dulls emotional pain. What I am offered is hope that together we can work to help me learn to manage my distress, make friends with my emotions and make changes to the behaviour which so far has served to prolong my suffering.
Throughout my experience of DBT I was encouraged to attend ‘training sessions’ (Group Skills) and apply those skills with the help of my DBT therapist (my ‘Coach’) to my own life. The question which after decades opened the door on hope for me, having ‘failed’ at numerous talking therapies, was ‘What does a life worth living look like for you?’ I was informed that no treatment or professional can undo my past experiences, nor can one person or therapy undo decades of maladaptive coping mechanisms in a limited period of time and within solely clinical settings. As with referrals to Physiotherapy for those with physical injuries, recovery means that there is a responsibility on the patient to take the exercises learned and practise them in the real life setting.
2. Managing Limits – From the beginning of the DBT therapeutic relationship, there is a clarity and agreement that both patient and professional will have their own personal and professional limits - it is helpful if an agreement is made about what those limits are and what the likely consequences of breaching those limits will be. There is also an understanding that each therapist has the backing of a team who understand and agree with the ethos of the DBT approach. This provides protection for both the patient and the therapist. In terms of carrying it into real life this models protective boundaries necessary to keep relationships going.
In the past my life patterns seemed to go in five year cycles. Every five years my central relationships would not only end, but explode with all kinds of collateral damage, resulting usually in a loss of accommodation and employment. I would spend some time in treatment, recovering, usually travelling abroad, in extreme settings (ie war zones), then restarting in a new location. Now I am building up a strong network of friends in a place I have lived and worked in for 16 years. When I was first diagnosed I was socially isolated and unable to find the emotional strength to start to build relationships outside myself and those necessary for a job to work.
3. Managing Reality – When struggling with the basics of life, usually most forcefully at the beginning of the recovery journey, before diagnosis, there is a perception that I am the only one experiencing life in this way. I have a distorted view of the levels of my own failures. In a sense I believe I was like Supergirl, not only did I feel I was an alien on earth, I also expected of myself massively higher standards and limits than anyone else. Until, ESPD became my ‘Kryptonite’ reminding me that after all I am flawed and human, and therefore absolving me of responsibility for everything bad in the world. In short, as I was reminded during my DBT journey, the universe doesn’t actually revolve around me and there are many, oh so many, things I do not and cannot control.
Another reality that comes as a shock after years of trying to manage a daily rollercoaster ride of extreme feelings is that, most of everyday life is boring and uninspiring - when struggling with Mental Health issues there can be a distorted view of life on the 'other side' where life must be rosy, easy and better than that experienced by me.
This is where involvement in real communities, becomes essential to maintaining recovery. If I can only relate to those who have an experience of Mental Health Services, or who have a shared diagnosis, then I am not allowing myself to experience the variety of relationships around me. It is more positive and more akin to real life to join groups which are focused on a location, sport, or interest. I have developed a ‘wellness group’ which, after nearly 3 years is firmly established within a defined local community. This means that we offer not only a weekly group focused on a programme to help us engage with activities which are available locally and can help our mental, physical and spiritual wellness. We have a strong online community of over 100 people who have come through word of mouth. We recognise that people are on a different part of the recovery journey so our weekly group is flexible and adapts to the needs of the group membership. As such we do not have a static membership, some people attend during sickness absences from work as a support in returning to work and move on. Some attend not knowing much about how to ask for help and need signposting and practical support to access GP referrals. Some are carers. Since we began we have had 50 members of the weekly group with this year’s group running at 6-8 people attending each week. We also meet on a one to one basis to provide signposting and advice, contact is usually made via local community contacts or by Direct Message on our Facebook page.
We encourage people to move out from our group and try other community involvement through our contacts with local groups and businesses. Having the opportunity to contribute within a wider community is vital to recovery. There is such a thing as a meaningful life - this cannot include unlimited access to Mental Health services as that is not the experience of most people. There is something intrinsically unhelpful if the only safe places a person feels they have can only be within Mental Health services or in socialising with those who have similar experiences. This is different from peer support.
4. Managing Discharge – From day one the end of DBT therapy and discharge were discussed openly with me, even though my actual date of discharge was nearly two years away, I was preparing for it from the moment I started therapy. Unlike my previous experience of endings I was more than ready to move forward, even though I was not symptom free I was able to leave feeling confident that I could live with the limits caused by my ‘Kryptonite’.
5. Managing my condition - Everyone has the ability to manage their condition if provided with the right skills and therapy to help them build a meaningful life in spite of their diagnosis. Hope is always there from day one underpinning the efforts of both staff and patients.
A Word about Relapse
I was discharged from the Complex Care and Treatment Team in 2014. In April 2017 I suffered a relapse in my condition requiring the intervention of the Crisis Team and Home Treatment Team. This had been triggered by financial pressures caused by a 2/3 cut in my benefits. Apart from not having enough for food and utilities this could have resulted in the repossession of my home. Thankfully the work I had put into building strong relationships meant that some friends were able to buy a percentage of my house and secure my residence. At the same time, it was taking 18 months to appeal the assessment decision. Each stage in the appeals procedure was highly distressing and only ended in October 2017 when I had to present my case to a panel at the Magistrates’ Court. Sometimes the environment is too powerful for me to manage even with my DBT skills.
I did feel like a failure, but I was told the DBT team within LCFT had developed the Acute Therapy Service (ATS) which helped me to stay in my home with the support of the HTT and my social network. I travelled to the ATS unit daily and for six days was given respite from the relentless pressures, to sharpen my mindfulness and emotion management skills. It felt like I was able to reboot and return to the same pressures but with my hope restored.
When you have been on the recovery pathway for some time, relapse can feel devastating until I take a step back and recognise how far I’ve come. The skills I once relied on to prevent self-harm are no longer required, but other sets of DBT skills are habitual, particularly mindfulness.
Hope and Meaning
Hope and Meaning cannot properly be provided by medication or therapy within a clinical setting. For me, hope and meaning come from a personal faith in a God who is bigger than me and my past and problems. For anyone, whatever their belief system finding someone or something that is bigger is important to providing an answer to the question, ‘What do you get up for each day?’ I think that the journey through therapy can partly be a search to discover what this is for each individual. It’s important for me to know why I should comply or co-operate with interventions or medications. In the past when I was unable to find an appropriate answer I was the nightmare patient – ‘uncooperative’ and ‘disruptive’.
I have long held that all of life is a journey, we pass through different terrain and places. Along our life’s journey we may be joined by others who travel the same path. I have seen those who have helped me as Care Co-ordinators, Therapists and Facilitators as ‘journey friends’, people who join me for a part of the journey. Some, the best practitioners, walk alongside me. Others, run ahead, leaving me lagging behind. Others, stay behind me, out of sight, making me feel uneasy and judged.
I am grateful for a therapeutic pathway which offered me hope that things could be different one day.
Sunday, 18 February 2018
Joy and the Emotionally Sensitive Person
'Sassy', I think this is one of my favourite words, and attitudes! There have been a large number of words used to describe me down the years: 'moody', 'drama queen', 'over sensitive', 'touchy', I could go on. However, the 'Sass' in me is fed up of the negative vocabulary attached to my diagnosis, that in itself seems confused. On my medical records the labels have changed from 'borderline', to 'emotionally unstable', to 'emotionally sensitive'. None really adequately conveys the reality of living in the emotionally sensitive skin.
As I progress in my recovery, I am beginning to find more positive words to describe my experience of life. When I see the worst in the world, the pain can almost certainly cause distress and unbearable pain. The flip side is that when I allow myself to focus on the good things in life, pleasant feelings are amplified into joy. I can really enjoy the small pleasures of life. Just as the pain and distress of life can be experienced by me to its depths, I am able to enjoy good feelings in wonderful technicolour. This is the freedom of owning my emotions and embracing the times of enjoyment, sometimes to the embarrassment of my companions. Dancing down the steps of the cinema, then taking a bow, following two hours of really enjoying a musical, is me allowing myself to express real joy, as much as I have let the reins go on my more destructive emotions. The difference is a little public expression of happy feelings is not destructive, in fact, perhaps my expression of strongly felt emotion was an echo of fellow cinema goers' enjoyment of the same film. The spontaneous applause from them as I skipped to the bottom step and turned round, was a moment of real shared joy, in a pretty unpleasant national and international setting.
I am good company, because I can take the smallest glimmer of enjoyment and amplify it (when I allow myself not to fear the strength of my positive emotions). Balance is important so that light feelings don't spiral out of control - but for too long the negatives of emotional sensitivity have led to me keeping my strengths in check.
I love the poem 'When I am Old I shall wear purple', except, now I'm 50 I'm not willing to wait until I'm old to embrace the best of my life experiences. Part of that is because I have allowed others to define what responses to my life are 'acceptable' for too long. The words I apply to me need to become: colourful, fun, strong, empathetic, sensitive to others, creative, optimistic - yes, really! I've realised recently simply because of my ability to come back from knockdowns and how I see what is possible, that I am an optimist. I believe in enjoying small pleasures just like a toddler - not out of control - but absolutely one hundred per cent, totally involving myself, body, mind and soul in enjoying the moment. Not childish, but childlike. It's no accident that the feel good clips most enjoyed on YouTube tend to focus on young children, kittens and puppies.
I'm currently watching the Winter Olympics and once again Elise Christie (GB Short Track Skater) has experienced unbelievable setbacks. One thing that a friend of hers said about her emotional responses struck me; she is able to embrace the pain and the feelings of despair so strongly, but unlike others, who can't do that, having faced the worst she can feel, she very quickly comes right back up again, ready to fight. Sometimes the emotional impact of the worst in life floors us for longer than we want. The fact that so many emotionally sensitive people face the worst thoughts and feelings about themselves and life, yet keep going, shows me there is always a seed of hope within. Building up the experiences of our most joyful moments, so they become a buffer against the bleaker times of life, helps us to be even more resilient than we give ourselves credit for.
As I progress in my recovery, I am beginning to find more positive words to describe my experience of life. When I see the worst in the world, the pain can almost certainly cause distress and unbearable pain. The flip side is that when I allow myself to focus on the good things in life, pleasant feelings are amplified into joy. I can really enjoy the small pleasures of life. Just as the pain and distress of life can be experienced by me to its depths, I am able to enjoy good feelings in wonderful technicolour. This is the freedom of owning my emotions and embracing the times of enjoyment, sometimes to the embarrassment of my companions. Dancing down the steps of the cinema, then taking a bow, following two hours of really enjoying a musical, is me allowing myself to express real joy, as much as I have let the reins go on my more destructive emotions. The difference is a little public expression of happy feelings is not destructive, in fact, perhaps my expression of strongly felt emotion was an echo of fellow cinema goers' enjoyment of the same film. The spontaneous applause from them as I skipped to the bottom step and turned round, was a moment of real shared joy, in a pretty unpleasant national and international setting.
I am good company, because I can take the smallest glimmer of enjoyment and amplify it (when I allow myself not to fear the strength of my positive emotions). Balance is important so that light feelings don't spiral out of control - but for too long the negatives of emotional sensitivity have led to me keeping my strengths in check.
I love the poem 'When I am Old I shall wear purple', except, now I'm 50 I'm not willing to wait until I'm old to embrace the best of my life experiences. Part of that is because I have allowed others to define what responses to my life are 'acceptable' for too long. The words I apply to me need to become: colourful, fun, strong, empathetic, sensitive to others, creative, optimistic - yes, really! I've realised recently simply because of my ability to come back from knockdowns and how I see what is possible, that I am an optimist. I believe in enjoying small pleasures just like a toddler - not out of control - but absolutely one hundred per cent, totally involving myself, body, mind and soul in enjoying the moment. Not childish, but childlike. It's no accident that the feel good clips most enjoyed on YouTube tend to focus on young children, kittens and puppies.
I'm currently watching the Winter Olympics and once again Elise Christie (GB Short Track Skater) has experienced unbelievable setbacks. One thing that a friend of hers said about her emotional responses struck me; she is able to embrace the pain and the feelings of despair so strongly, but unlike others, who can't do that, having faced the worst she can feel, she very quickly comes right back up again, ready to fight. Sometimes the emotional impact of the worst in life floors us for longer than we want. The fact that so many emotionally sensitive people face the worst thoughts and feelings about themselves and life, yet keep going, shows me there is always a seed of hope within. Building up the experiences of our most joyful moments, so they become a buffer against the bleaker times of life, helps us to be even more resilient than we give ourselves credit for.
Tuesday, 6 February 2018
Groundhogs and Finding the Words
Groundhog Day is a bizarre American public holiday based around the behaviour of a brown, furry rodent, upon which the nation apparently bases its expectation for how much longer winter will last. Until the release of the film 'Groundhog Day', so far, so obscure. Now, we use the phrase to mean recurring events or conversations. Over the past two weeks, I've had that sense of 'Groundhog Day' as I have had conversation after conversation on the same lines. 'My husband/partner/brother/sister/friend/carer keep asking me how they can help me, they keep asking, how they can 'fix' me.'
It's a familiar conundrum, we wish we felt loved, but need to know that with love comes a desire to do 'something' to take the pain and hurt from us. For us, the issue is to prevent pushing the love away with the offer rescue. So often, the conversations continue, 'I wish (he/she) knew that all I want is a hug and reassurance.' So often, it seems that even to find a way to say something this simple is so hard.
I'm no expert, but I have gleaned some wisdom from those who have managed to voice their thoughts to their loved ones and found a way forward together.
1. If You Can't Say it, Try Writing It. Write a letter to your loved one and pin it to the family memo board, or to the fridge, or on the loo door; somewhere they can't miss it.
2. Relieve Them of The Duty to Be Your Saviour. I've stated before that it is an impossibility for one person to provide all of our emotional needs. Those closest to us need to know that we don't expect them to rescue us. Just as I have to accept that I can't rid myself of all pain, so I need to absolve those closest to me from the pressure of believing they have to take the pain away from me. Together we need to work together - I have lived my life, survived my trauma. I do not need to share the fallout from those past experiences as a burden on my current relationships. What I would welcome is someone to walk alongside me, to build me up with present positives, particularly when carrying the burden of my condition or my past wears me down. In the healthiest ways possible I need my current relationships to be nurturing and equal.
3. Be honest. Express to them what other things, practical things would really help when you are feeling overwhelmed. For example, it's okay for children to spend one to one time with a parent if that allows time for the other parent to restore batteries. Support one another in becoming involved in social and other positive activities outside the home. Empty vessels have nothing to offer others.
It's a familiar conundrum, we wish we felt loved, but need to know that with love comes a desire to do 'something' to take the pain and hurt from us. For us, the issue is to prevent pushing the love away with the offer rescue. So often, the conversations continue, 'I wish (he/she) knew that all I want is a hug and reassurance.' So often, it seems that even to find a way to say something this simple is so hard.
I'm no expert, but I have gleaned some wisdom from those who have managed to voice their thoughts to their loved ones and found a way forward together.
1. If You Can't Say it, Try Writing It. Write a letter to your loved one and pin it to the family memo board, or to the fridge, or on the loo door; somewhere they can't miss it.
2. Relieve Them of The Duty to Be Your Saviour. I've stated before that it is an impossibility for one person to provide all of our emotional needs. Those closest to us need to know that we don't expect them to rescue us. Just as I have to accept that I can't rid myself of all pain, so I need to absolve those closest to me from the pressure of believing they have to take the pain away from me. Together we need to work together - I have lived my life, survived my trauma. I do not need to share the fallout from those past experiences as a burden on my current relationships. What I would welcome is someone to walk alongside me, to build me up with present positives, particularly when carrying the burden of my condition or my past wears me down. In the healthiest ways possible I need my current relationships to be nurturing and equal.
3. Be honest. Express to them what other things, practical things would really help when you are feeling overwhelmed. For example, it's okay for children to spend one to one time with a parent if that allows time for the other parent to restore batteries. Support one another in becoming involved in social and other positive activities outside the home. Empty vessels have nothing to offer others.
Subscribe to:
Posts (Atom)
-
Emotions for most people naturally seem to come and go. Most people experience either euphoria, grief or anger as passing extremes. For me, ...
-
"When you need me, but don't want me, then I'll stay. When you want me, but don't need me, then, I'll have to go"...
-
'Treating someone with borderline personality disorder can be one of the toughest challenges a [social worker] encounters. Life for suc...